Background
Patient Name: Charlotte
Condition: Complex Lower Limb Deformity
Age Range Covered by Case Study: 14 years to 16 years
Abstract
Charlotte has been my patient since she was three years old. Over the years, I’ve collaborated with other medical professionals to treat her for various issues with her right leg.
Her issues began with a hemangioma that involved her entire right tibia. The hemangioma damaged her knee, ankle, and foot joints in addition to her growth plates which inhibited the growth of new bone. After several minimally invasive procedures, the hemangioma was finally stabilized when she was eight years old.
At the age of 11, Charlotte underwent osteotomies and plates were put in place to treat rotational and angular deformities that had developed in her leg and foot.
Charlotte later suffered fractures in her fibula and tibia and the rods from the osteotomies had to be removed because the hemangioma had caused her bones to shift out of position and the rods to protrude causing pain. Delayed bone growth caused by the hemangioma resulted in a large limb length discrepancy (over three inches). At the age of 13, we discussed the option of surgically correcting her limb length discrepancy and deformity with a Taylor Spatial Frame.
Treatment
SURGERY #1
- Removal of Lock Plate from the Proximal TibiaAn incision was made over the proximal tibia at which point the lock plate was found and the plate along with all screws were removed.
- Removal of Intramedullary (IM) Rod from TibiaThe IM rod was located within the tibia but could not be easily removed. A surgical drill was used to cut the IM nail and to saw the rod into pieces that could be more easily removed in parts.
- Proximal & Distal Tibia Deformity Correction & Lengthening w/ Application of Taylor Spatial FrameA Taylor Spatial Frame was applied in a bifocal manner with three rings and six struts. The tibia was noted to be quite small and abnormal due to distal deformities that caused the bone to bend outwards (valgus) and inwards (varus) along with a severe proximal deformity where her knee bent backwards (recurvatum). In a rather complicated procedure, osteotomies were performed both proximally and distally as I tried to achieve approximately 5cm (2in) of increased length.

Charlotte in the hospital after having her Taylor Spatial Frame applied.
Post Op
Charlotte was given schedules for adjusting the struts of the frame to create space and allow the bone to grow.

Charlotte’s mom inspects her Taylor Spatial Frame.
Observations
Two weeks after surgery, her sutures were removed and all pin sites were found to be clean. A week later, there was good range of motion in her knee and foot. X-rays revealed the tibia was lengthening well and in proper alignment.
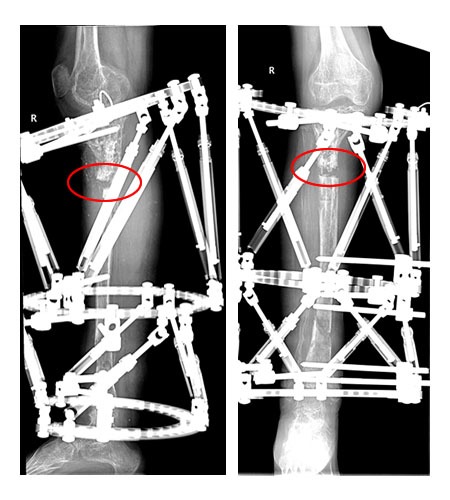
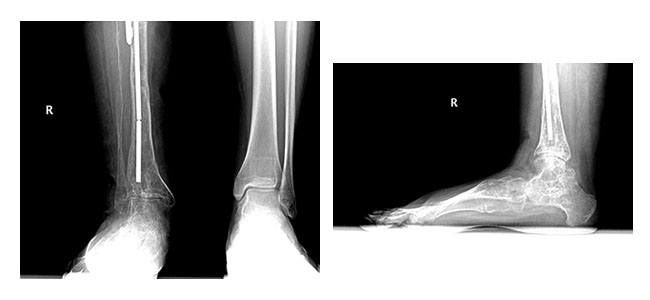
X-rays of Charlotte’s right tibia three weeks after having her TSF applied.
Over the next few weeks, various struts in the upper and lower frames were changed to accommodate the new length of the limb.
Four months after surgery, the regenerated bone at the distal tibia osteotomy site appeared to have healed. However, the union of the regenerated bone at the proximal tibia osteotomy site was delayed. Plans were made to remove the distal frame and inject the proximal tibia site with bone marrow to promote bone growth.
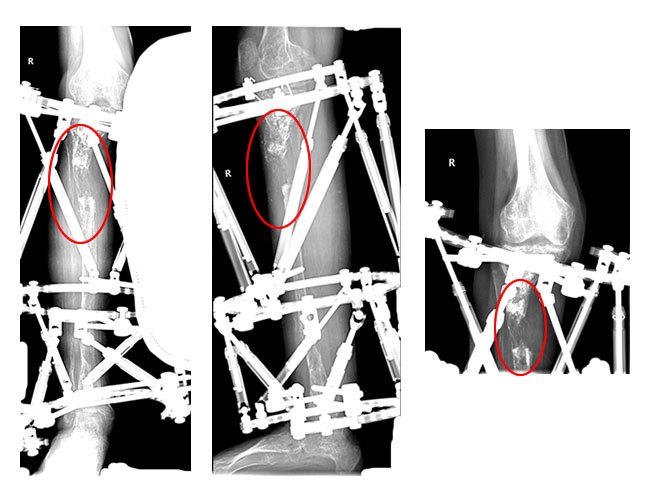
An x-ray of Charlotte’s tibia four months after her osteotomy. Note the regenerated bone at the proximal osteotomy site is not united.
SURGERY #2
- Injection of Bone Marrow Aspirate, Demineralized Bone Matrix into Delayed Union of Lengthening
A few struts were removed from the distal frame to allow for examination of the osteotomy site to determine if it had healed. A Jamshidi needle was used to draw 20cc of bone marrow from the right iliac crest. The bone marrow was then mixed with demineralized bone matrix and dye (Hypaque). 16cc of the bone marrow mixture was injected into the proximal delayed nonunion site and 2cc were injected into the distal site.
- Removal of Wire From Proximal Tibia
The entire frame was left in place but some of the transfixion wires were removed from the proximal tibia.
Observations
Two months after surgery, x-rays revealed insufficient bone formation. It was decided that a bone graft would be performed.
Insufficient bone formation at the proximal osteotomy site.
SURGERY #3
- Iliac Crest Graft & Infusion of Bone Morphogenetic Protein (BMP7)
The distal tibia osteotomy site was tested and noted to be moving, indicating there was still a nonunion. An incision was made over the posterior iliac spine and a graft was taken from the iliac crest. Another incision was made over the nonunion distal site, the nonunion tissue and bone was debrided, and the iliac crest graft and BMP 7 were applied to the area. This procedure was repeated at the proximal nonunion site.
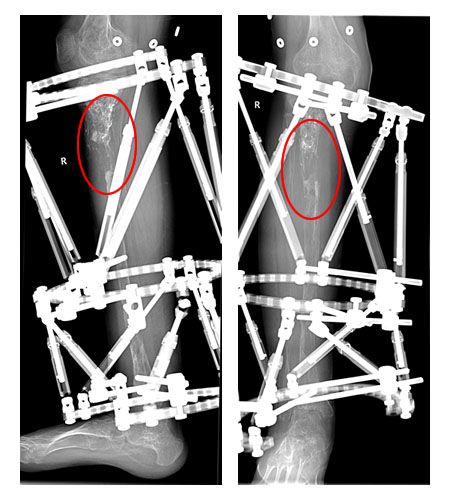
X-ray of tibia two weeks after bone graft and BMP7 infusion.
Observations
Charlotte made one emergency visit to the office due to swelling in her right knee. The combination of having her leg extending for a long period of time while being fitted for a new brace and then extensive walking around school placed a lot of stress on her knee which resulted in swelling. However, there was no need for intervention beyond elevating and icing the leg while at rest.
SURGERY #4
- Hardware RemovalA check was performed to ensure that there was continuity of the bone within the tibia. The Taylor Spatial Frame was then removed, all pin sites were debrided, and Charlotte’s leg was placed in a short-leg cast. The bone was thin but appeared intact and x-rays showed good positioning.
Observations
One month after surgery, x-rays showed no major changes from previous x-rays but a small area of buckling at the proximal tibia was of some concern. Charlotte’s short leg casts were replaced with new waterproof casts and she was able to place full weight on the leg.
SURGERY #5
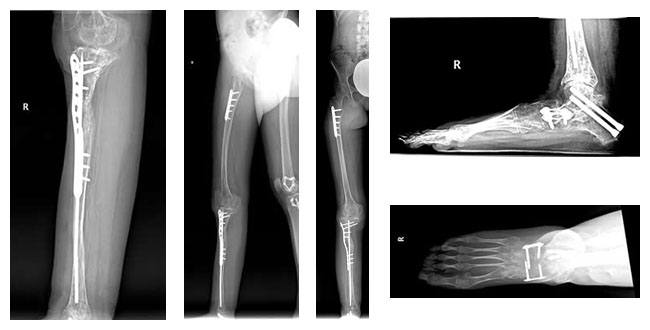
- Open Reduction Internal Fixation (ORIF) with William’s Nail & Synthes Locking PlateAn incision was made over the nonunion and proximal tibia. The bone edges were aligned and a Williams rod and small plate were used to hold the previous area of nonunion in place.
- Infuse at the Tibial Nonunion SiteBMP7 was used at the nonunion site to stimulate healing of the bone. Charlotte’s leg was then placed in a bivalved long-leg cast.
SURGERY #6
- Change of Plaster & Manipulation Right Foot with Long Leg CastingCharlotte was taken back into the operating room and her stitches and cast were removed. The wound was clean and completely healed with no signs of infection. The osteotomy, fracture, and nonunion sites appeared to be in good position and healing/strengthening. Dressings and a long leg cast were applied.
Observations
One week after surgery, Charlotte’s leg cast was shortened to below her knee to allow for bearing weight on her right leg.
Four months after surgery, x-rays showed excellent bone formation in the tibia and that all hardware was in place. Plans were made for Charlotte to walk at home with her brace and no crutches and then without braces or crutches.
Five months after surgery, x-rays revealed excellent bone formation and a normal ankle. However, there was severe arthritis and a deformity in the subtalar joint which caused severe pain when the joint was moved. It was decided that Charlotte would wear a Jobst stocking for support and continue physical therapy. Her foot would be reevaluated in six months at which point triple arthrodesis would be considered if there was no improvement.
SURGERY #7
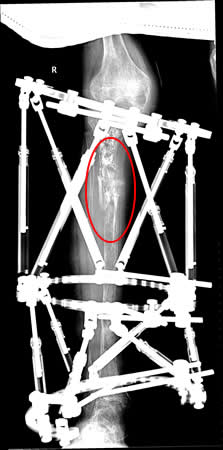
An x-ray of Charlotte’s ankle five weeks before her seventh surgery.
- Triple Arthrodesis of the Right Foot & Ankle Including the Subtalar, Calcaneocuboid, & Talonavicular Joints with Plates & Screws Utilized for Fixation
An incision was made over the joint between the ankle and heel (sinus tarsi) and clear liquid flowed from the wound as a result of a hemangioma on the foot; a tourniquet was applied. At this point, cartilage was stripped (denuded) from the medial and posterior facets of the joint (arthroplasty).
The talonavicular and calcaneocuboid joints were then opened with a closing wedge osteotomy on the talonavicular joint. An opening wedge osteotomy was performed at the calcaneocuboid joint. Arthroplasties were performed on all of the joints. Next, a plate was inserted into the talonavicular joint and screws were then applied to the calcaneocuboid joint. A bone transplant (allograft) was then applied to the calcaneocuboid joint and held in place with a plate and screws. Good fixation was achieved and Charlotte’s foot and all hardware were in proper position.
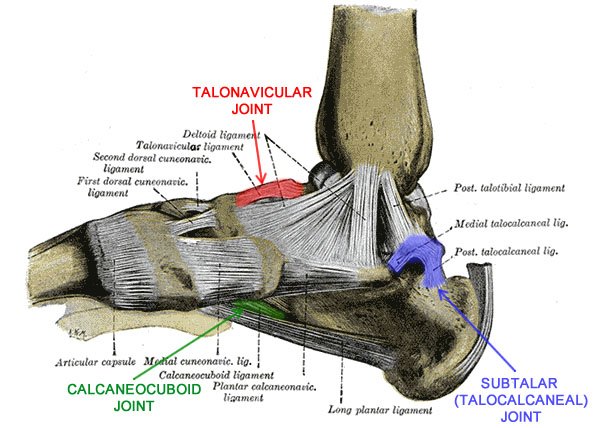
Joints fused during Charlotte’s triple arthrodesis procedure.
SURGERY #8
- Change of Plaster & Removal of SuturesAll wounds were found to be dry and clean and sutures were removed. Dry sterile dressings were applied and short-leg casts were reapplied.
Conclusion
Charlotte is doing well overall and is actively involved with sports. I’ve recommended a 1cm shoe lift for better balance and symmetry in addition to ongoing physical therapy for strengthening which will allow her to eventually walk without her crutch. While it’s possible that Charlotte’s lower right limb may never be as strong as her left, treatment has allowed her to avoid the need for an above knee amputation and prosthesis. This case is an example of multiple complex factors requiring an extended course of treatment that is now concluding with a well functioning limb.
From My Patient
I was only 3 years old when I met Dr. Feldman. My parents and I had seen many doctors and it was discovered that I had vascular tumors in my tibia. These vascular tumors left a hole at the top of my tibia and caused the remaining half of my bone to be honeycombed. All doctors wanted to operate on my leg except Dr. Feldman. He was able to determine that the tumors were inactive. Instead of putting me through multiple surgeries at such an early age, Dr. Feldman decided that the best course of action was to fill in the hole and to monitor me. For the next seven years I was able to walk and run around without any surgeries. By the age of ten these vascular tumors had once again become active and this time had damaged my growth plate. My tibia rotated 50 degrees out and my femur turned 30 degrees in. When I could no longer walk Dr. Feldman went in to correct the deformity by breaking and reseting my femur and tibia. During this operation Dr.Feldman was able to realign my leg. Unfortunately the damage to my growth plate was so severe that in the coming years it became evident that I was not growing in my right leg.
Two years ago Dr.Feldman performed a limb lengthening and realigning of my right tibia. I had a two and a half inch discrepancy between my legs and the rod in my tibia was bent back behind the knee. Dr.Feldman had to remove all existing hardware in my tibia and then attach a Taylor Spatial frame to my leg. This frame both realigned and lengthened my leg. Although the lengthening process was very long, it was definitely worth it. It felt odd having an extra 4 pounds attached to my leg, but I learned to live with the frame and it lengthened my leg 2 and a half inches! That in itself is a miracle and is all thanks to Dr.Feldman. Over the course of 13 years I have undergone multiple surgeries to correct the deformity in my right leg. Today that deformity no longer exists because of Dr. Feldman.
No Guts No Glory.

After living with a Taylor Spatial Frame on my leg for 13 months, I discovered how hard it is to fit clothes over the frame. Going through this process inspired me to create my own clothes. While in the frame, I wore skinny jeans that I had designed to fit over the frame because I didn’t want to wear baggy clothes. Having a Taylor Spatial Frame on has its own challenges that one should not have to worry about the difficulty of clothes. I am in the process of designing a clothing line and am starting with the very basics-underwear for girls(guys are next). After going through this process myself I quickly learned basic underwear didn’t fit over the frame and velcro didn’t seem to work. That is why I have designed underwear with snaps on the side that are fashionable,comfortable, and easy to put on. I am in the process of launching my underwear line which not only caters to individuals with a Taylor Spatial Frame, but to anyone who may not have full mobility. The name of my clothing line is “No Guts No Glory” because it takes guts in order to achieve the glory of success.If you’d like to contact me with any questions and or would like to purchase this underwear my website is www.crnogutsnoglory.com.
Check out my website for tips on healing a taylor spatial frame including cleaning suggestions, what to expect after surgery and to hear my full story.
Image courtesy - www.feldman.vwmdev.com






